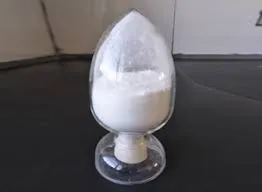
Pentoxifylline A Comprehensive Overview
Pentoxifylline is a methylxanthine derivative, primarily known for its vasoactive properties. It is commonly used to improve blood flow in patients with conditions that impair circulation, such as peripheral artery disease (PAD) and diabetic ulcers. This article aims to provide a comprehensive overview of pentoxifylline, including its mechanism of action, clinical applications, side effects, and considerations for use.
Mechanism of Action
Pentoxifylline is classified as a phosphodiesterase inhibitor, which leads to an increase in intracellular cyclic AMP (cAMP) levels. The rise in cAMP facilitates vasodilation, improving blood flow to affected areas. Additionally, pentoxifylline enhances the flexibility of red blood cells, enabling better transportation of oxygen to tissues. This dual action of improving blood flow and oxygen delivery makes pentoxifylline particularly useful in treating conditions associated with poor perfusion.
Clinical Applications
Pentoxifylline is primarily prescribed for the treatment of intermittent claudication, a painful condition that occurs when the legs do not receive enough blood during physical activity. Patients with PAD experience reduced blood flow, leading to pain and discomfort, which can limit mobility. Studies have demonstrated that pentoxifylline can reduce symptoms and improve walking distance in these patients.
Beyond claudication, pentoxifylline is also utilized in the management of diabetic foot ulcers and venous leg ulcers. Its ability to enhance microcirculation supports wound healing and reduces the risk of infection. Some clinicians also consider pentoxifylline for conditions involving chronic liver disease, such as hepatitis C, where it may improve liver function by enhancing blood flow to the organ.
define pentoxifylline
Side Effects
While pentoxifylline is generally well-tolerated, it can cause a range of side effects. Commonly reported adverse effects include gastrointestinal issues such as nausea, vomiting, and diarrhea. Some patients may also experience headaches, dizziness, or skin rashes. Rarely, severe adverse reactions such as bleeding or thrombocytopenia (low platelet count) may occur, necessitating careful monitoring of patients with pre-existing bleeding disorders or those on anticoagulant therapy.
Considerations for Use
Before prescribing pentoxifylline, healthcare providers should conduct a thorough assessment of the patient's medical history and current medications. Special caution is warranted for patients with a history of arrhythmias, as pentoxifylline may exacerbate certain heart conditions. It is also essential to consider potential drug interactions. For example, the concomitant use of other anticoagulants can increase the risk of bleeding.
Additionally, while pentoxifylline is effective in managing specific conditions, it should not be viewed as a standalone therapy. Lifestyle modifications, including smoking cessation, exercise, and dietary changes, play a critical role in managing peripheral artery disease and associated complications.
Conclusion
Pentoxifylline represents a valuable pharmacological intervention for improving blood flow and enhancing tissue oxygenation in patients with circulation-related issues. Its application in intermittent claudication, wound healing, and potentially in managing chronic liver disease highlights its versatility. However, like all medications, it must be used judiciously, taking into account the individual patient's profile and potential risks. As ongoing research continues to explore its therapeutic benefits, pentoxifylline remains a significant option in the arsenal against vascular diseases.

